A sleep doctor on the insomniac’s journey: and a possible shortcut
Insomnia is the most common sleep complaint. In any one year, 30% of us will have some difficulty sleeping, and one third of that group will have a problem that continues. Many unwanted outcomes can potentially follow. These include some very obvious to the sufferer—fatigue, concentration problems and memory impairment with important domino effects on family life and work—but also longer term risks including impaired immune function; physical health problems such as a tendency to higher blood pressure, and, in experimental situations of restricted sleep at least, diabetes.
And it’s not just physical health, insomnia can even lead to mental health problems such as depression, in fact, in some cases insomnia can be the first symptom of a later depression. In the journey the typical sufferer takes, there is a long period of denial, of believing that things will get better, but when they don’t, the search for remedies begins. The first remedy many people reach for is over the counter, whether that be valerian, antihistamines, or some other mild treatment. These have some, albeit limited, effect so people often find themselves reaching for something stronger: prescribed sleeping tablets. These are taken by a staggering 15% of the US population and come with a myriad of side effects. Memory impairment is possible, along with a morning hangover effect and potential effects on driving (to work, notwithstanding any alcohol consumed as well). And with some people, sleepwalking is provoked and an equivalent condition called sleep eating. So what on earth can be done to avoid these outcomes? An accepted tool with solid evidence to support it is called Cognitive Behavioural Therapy for insomnia, CPTi. Some of the techniques used in this therapist-guided approach to sleep hygiene are limiting late caffeine, exercising, avoiding the use of electronic devices in the bedroom because of light exposure, and keeping the bedroom cool and quiet. The most powerful technique may be restricting the amount of time spent in bed, as most insomniacs spend too much time actually in bed. Access to this therapist-guided treatment is likely to be limited and results may be a long time coming. So what can people do on their own? Sleep hygiene will always be relevant, as will going to bed later, but more importantly, employing mindfulness has proven consistently effective. More and more studies show the benefits of beginning a meditation practice to help with sleeping. As a self-directed non-drug treatment, it’s an easy place to start. Putting intrusive thoughts to rest is clearly likely to help, as a “chattering mind” is common in insomnia. If meditation is practiced at an earlier stage in the insomniac’s journey, it may be shortcut that avoids some of the poor outcomes mentioned above.

Be kind to your mind
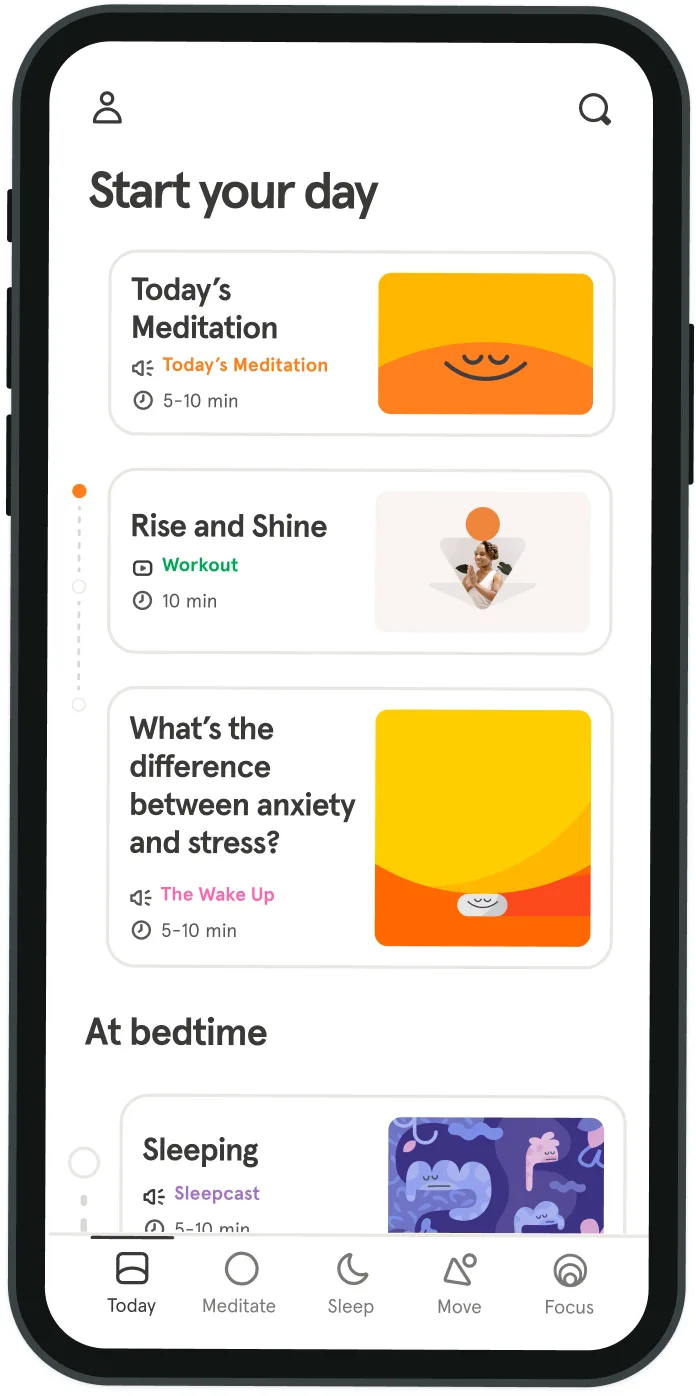
- Access the full library of 500+ meditations on everything from stress, to resilience, to compassion
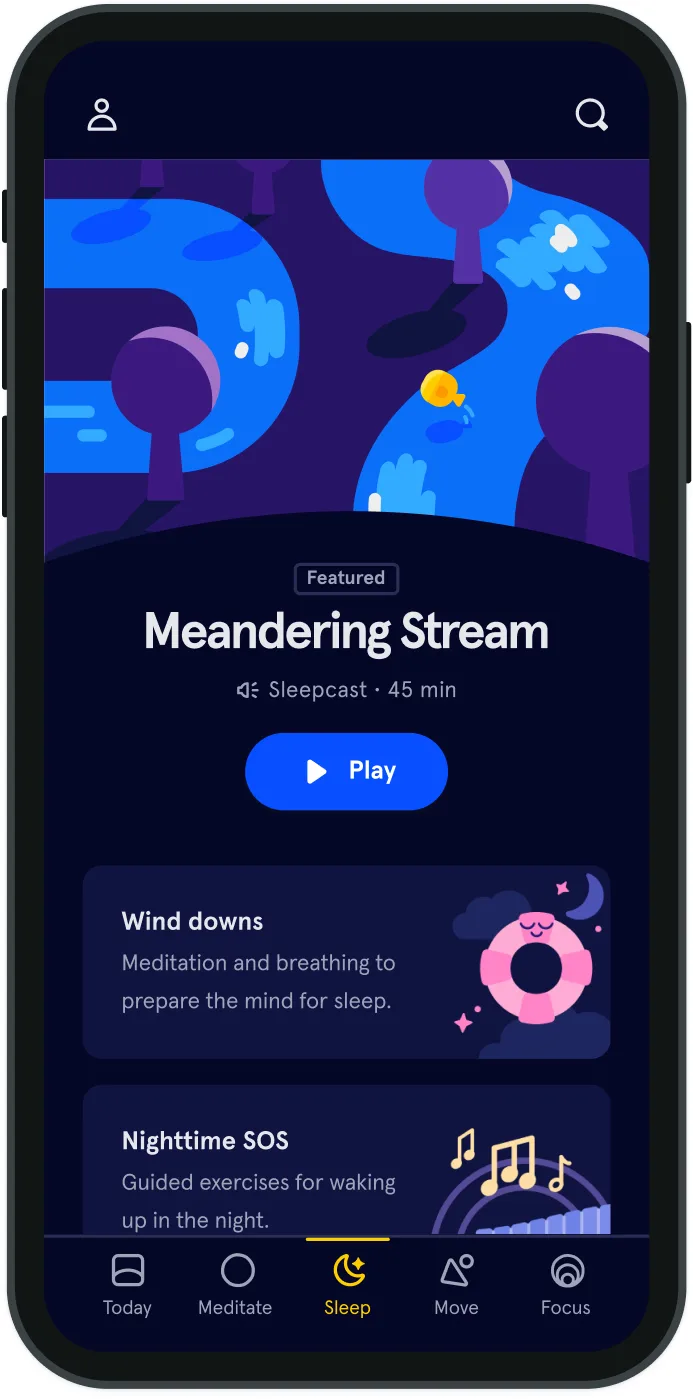
- Put your mind to bed with sleep sounds, music, and wind-down exercises
- Make mindfulness a part of your daily routine with tension-releasing workouts, relaxing yoga, Focus music playlists, and more
Meditation and mindfulness for any mind, any mood, any goal
- © 2024 Headspace Inc.
- Terms & conditions
- Privacy policy
- Consumer Health Data
- Your privacy choices
- CA Privacy Notice
